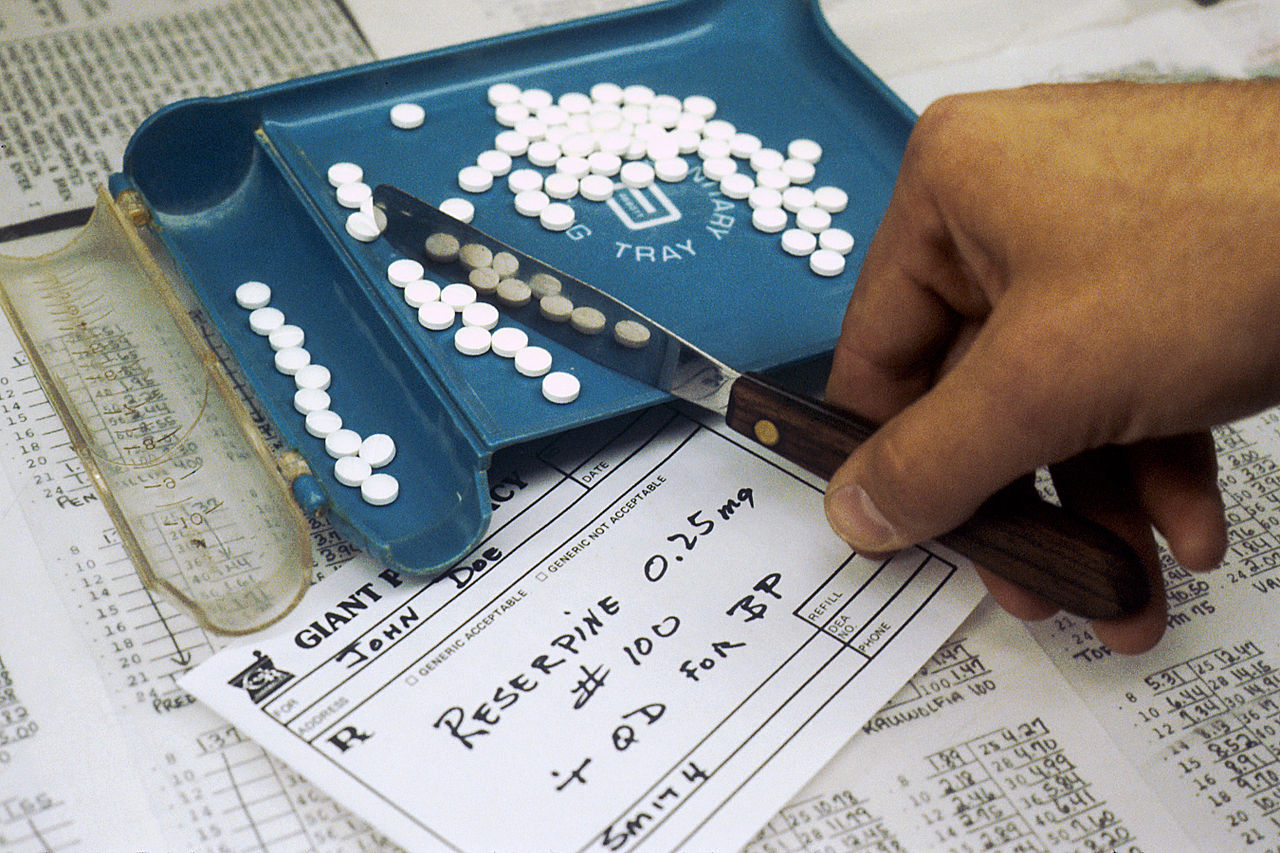
Where Your Doctor Went To School Could Change How They Prescribe Opioids

By:
Ground zero of the opioid epidemic isn't seedy back-alleys or substance-fueled college parties—it's the doctor's office.
And new research suggests that doctors' schooling plays a significant factor is how likely they are to prescribe the drugs that most commonly trigger opioid addiction.
 Wikimedia - wikimedia.org
Wikimedia - wikimedia.org
Molly Schnell and Janet Currie, economists specializing in health care policy at Princeton University, set out to explore that relationship in a working paper published by the National Bureau of Economic Research this month. What they found was that physicians are significantly more likely to prescribe opioids if they graduated from lower ranking medical schools.
How much more likely? Compared to doctors who graduated from top institutions such as Harvard Medical School, doctors from lower-ranked schools "prescribe nearly three times as many opioids per year," the paper determined.
 Wikimedia - wikimedia.org
Wikimedia - wikimedia.org
It's a stunning difference that raises questions about how institutions are training physicians before they enter the field, prescription pad in hand. ATTN: talked to Currie about the paper's findings and where they see this research fitting into the broadening conversation around the nation's opioid crisis.
ATTN: What's the central finding from your team's research?
Janet Currie: The main takeaway is that there is a strong relationship between the rank of a doctor's first medical school and their prescribing behavior when it comes to opioids. There's some related facts in the paper, too. For example, a lot of doctors practicing in the U.S. were trained outside of the country and their prescribing patterns varies a lot by what region they were trained in. Those facts lead us to think that it's something about the doctor training that causes people to prescribe differently.
 Flickr - flickr.com
Flickr - flickr.com
ATTN: How does the relative ranking of medical schools account for differences in prescribing practices?
JC: I don't think it's necessarily that people at higher ranked medical schools are getting more specific training in opioids or pain medication. I think, though, that they might possibly be getting more evidence-based training or more emphasis on the fact that doctors can inadvertently do harm if they're not careful. They might have more resources to look up something or ask somebody if they were uncertain about it. They might be more likely to keep up with the literature after they leave.
There's a lot of different factors that could be responsible, and I have to be entirely upfront, we're not looking at any details of how people are trained, and it's not even clear to me how you could do that. Collecting data on all of these doctors over a long period of time on all the aspects of their training would be a really big job.
ATTN: What did you learn from doctors trained in different regions of the world?
JC: What's interesting there is how variable the trends are. On average, all foreign doctors together looked like medium-ranked U.S. schools, but doctors trained, for example, in the Caribbean have much higher opioid prescribing rates than doctors trained in Eastern Europe. It seems to me that very likely reflects differences in attitudes, which come from their backgrounds in training.
 Pixabay - pixabay.com
Pixabay - pixabay.com
ATTN: How did you factor in the parts of the U.S. where doctors were practicing, considering varying rates of opioid addiction across the country?
JC: In our statistical model, we actually controlled for that. In some of our models, we're basically looking at doctors from different ranked schools who practice in the same county and we're showing that there's still a difference. In some of our models, we even look at people who are practicing at the same address—for example, at the same hospital—and show that there's differences in their prescribing practices, which are related to what type of medical school they went to.
ATTN: Is it fair to say that we've underestimated the role of physician training in the opioid epidemic?
JC: I think it's been underreported. If you think about what are the things that get a lot of attention, one of them is treatment—how we need to have more treatment and is the treatment effective and so on, that's very important. Another one, people often, when they're thinking about opioids, go right to the illegal ones; so then they start talking about fentanyl or things from China or heroin—they go right to the illegal [opioids], and certainly that's a big problem. But a lot of the discussion sort of glosses over the fact that many people who become addicted, and even many of the people using heroin, started with prescription pain medications that were given to them by their doctors and then ended up being addicted.
I think we do need to think about that a lot more and talk about how to prevent that and when opioids are appropriate and when they're not appropriate. Some of the basic research suggests that opioids are not even very effective for chronic pain, outside of a palliative care setting, because people build up dependence, right? So it takes more and more opioids to get the same effects, and you have someone who started off with chronic back and they end up with chronic back pain plus addiction.
This interview has been lightly edited for length and clarity.
