How This Woman's Period Pain Story Reveals the Problem in Women's Health

By:
A woman's story about her unsuccessful efforts to obtain treatment for her severe period pain is creating buzz by highlighting how gender biases severely impact women's health.
Writing for Quartz, Olivia Goldhill explains that even though she told doctors her period pain was just as debilitating as having a slipped disc, they did not know how to treat her condition.
 YouTube/www.endofound.org - youtube.com
YouTube/www.endofound.org - youtube.com
"Every month I spent hours lying on the floor, unable to move, and literally crying out in agony. My hip and back muscles went into spasm, so that my body was twisted in an S-shape contortion whenever I stood—a condition that didn’t disappear when my bleeding ceased, but had to be treated with visits to a physiotherapist every four weeks." — Goldhill, Quartz
Not only that, but Goldhill's doctors repeatedly downplayed her pain.
"Before I had my MRI scans, I told my primary care doctor that the pain seemed to be triggered by my period. He didn’t think this was relevant and ignored the comment. Later, when scans showed my discs were in place, the specialist said my pain was likely due to nerve inflammation—just one of those painful things that someone with my history would likely suffer from time to time. Once again, his eyes flicked to the side and he waved his hands dismissively when I asked if it could be connected to my menstrual cycle." — Goldhill, Quartz
Goldhill faced similar circumstances when she visited her gynecologist, who said her pain was "normal" and that she "shouldn't be overly worried."
Goldhill even tried birth control pills to offset the symptoms but the overwhelming pain continued.
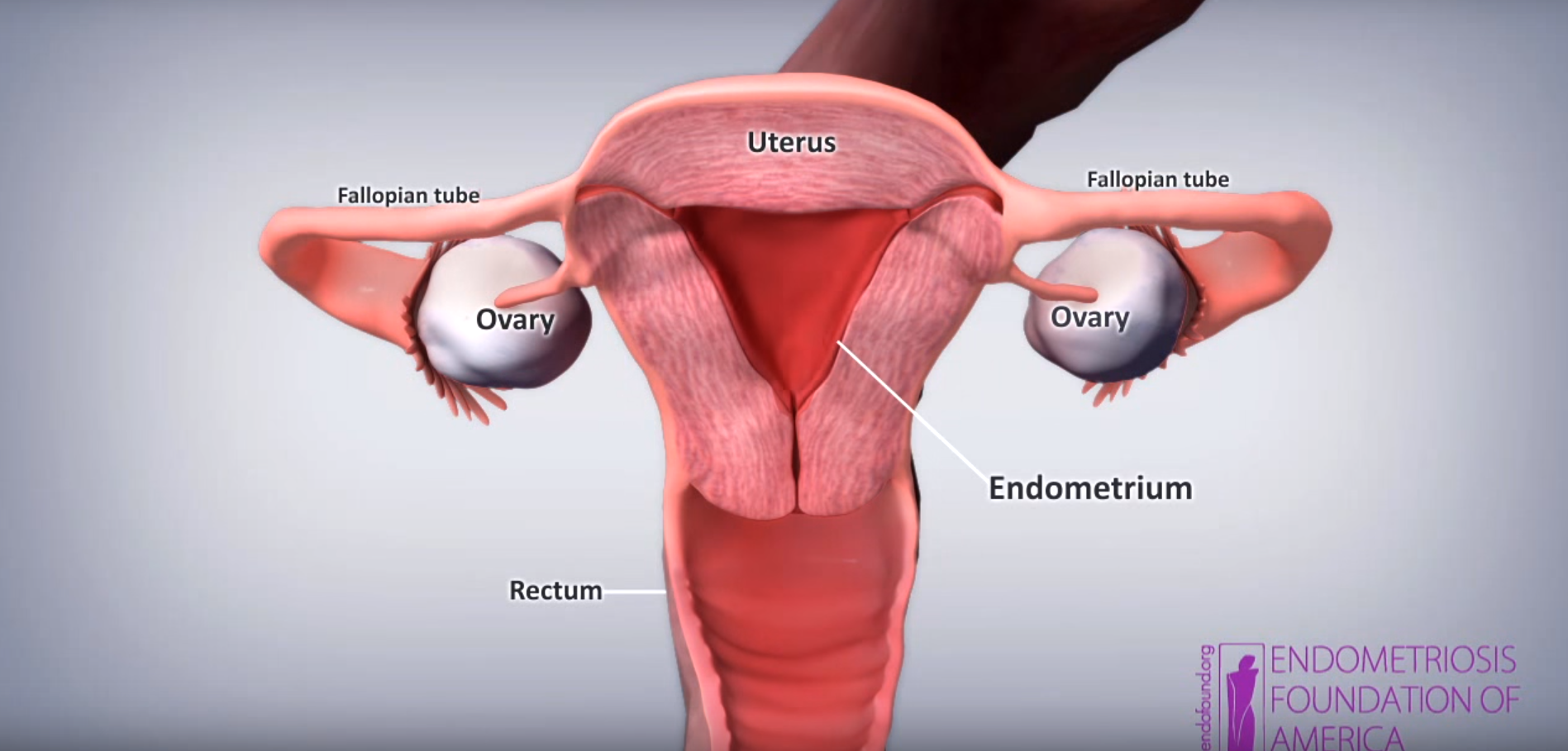
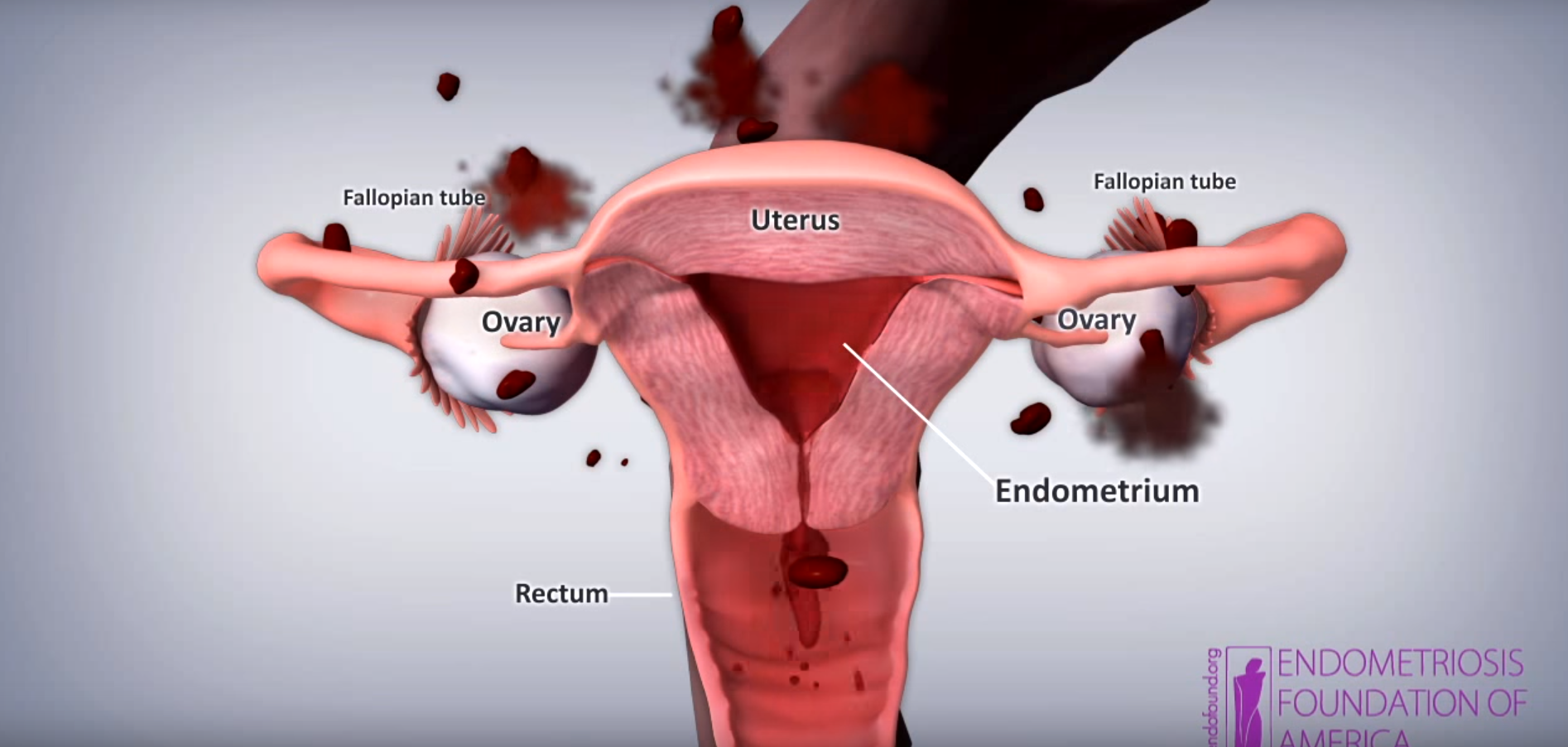
However, after doing some research of her own, Goldhill concluded she had endometriosis, a condition where tissue lining the uterus is found in other parts of the body such as the fallopian tube and the ovaries, according to the Endometriosis Foundation of America.
Though the symptoms vary, endometriosis causes very painful menstrual cramps that cannot even be treated by anti-inflammatory drugs. It also causes abnormally long periods, bowel and urinary disorders, nausea, vomiting and infertility. It affects 5 million women in the U.S. and 176 million women worldwide, yet the condition remains a mystery to doctors, and women are poorly treated for the condition according to the Guardian.
 YouTube/www.endofound.org - youtube.com
YouTube/www.endofound.org - youtube.com
The Guardian further reports that endometriosis has resulted in broken marriages, depression and an $80.4 billion hole in the U.S. economy from women leaving the workforce because of their symptoms.
Due to the lack of research, doctors tend to downplay the pain of endometriosis as nothing more than an especially painful period that a woman may not be accustomed to experiencing, according to Heather Guidone, the surgical program director of the Center for Endometriosis Care in Atlanta.
“Pain is never normal,” Guidone told the Washington Post. “A lot of society tends to dismiss pelvic pain, particularly when associated with a period. It may be acknowledged, but women are told that this is your lot in life for being female. They’re told they’ll grow out of it. They don’t.”
According to the Guardian, doctors often either accuse women of "imagining" the pain or that they simply "must put up with it."
In an article posted on BuzzFeed, 18 women talked about their struggle to receive a proper diagnosis for their case of endometriosis.
One woman said, "my doctor believed that I was lying about the pain for years just to get drugs.”
Another added, "it took four years of being called a hypochondriac before I was diagnosed.”
But this phenomenon of women's pain symptoms being ignored by doctors isn't limited to endometriosis. According to a study conducted at the University of Maryland, "women report more severe levels of pain, more frequent incidences of pain, and pain of longer duration than men, but are nonetheless treated less aggressively."
But why does this happen?
Part of the lack of seriousness toward women's health issues could be due to the "overly emotional" female stereotype.
According to the Huffington Post, the first mental disorder diagnosed in women was hysteria. It included hallucinations, emotional outbursts, nervousness and different sexual urges. Up until the 1950s, the idea of "female hysteria" was embraced by the medical community.
The dismissal of serious physical pain endured by women can have grave and permanent consequences. In the 1800s, female hysteria was often treated with a hysterectomy — a surgical procedure that removes a woman's uterus. As the blog Feministing explains, though hysterectomies have evolved as a way to treat serious health problems affecting the womb, it was once thought to be the cure for women who did not match female gender expectations:
Hysterectomies are an old and time honored surgical practice. Back in the 1800’s, hysterectomies were performed as a treatment for female hysteria. Hysteria was a diagnosis commonly given to women who were too loud, too quiet, too sexual, not sexual enough, ate too much, ate too little, too smart, too dumb, too tall, too short, and, in general, did not fit the mold for the “perfect woman.” So hysterectomies have been around for a long time, and have not always been performed for the best reasons. — Feministing
A 2008 study seemed to support the notion that gender biases played a role in emergency treatment for abdominal pain.
The study's authors found that although men and women had the same level of pain, women were less likely to receive analgesic treatment. And after factoring in race, age, triage, class, and pain score women were still 13 percent less likely to receive Opioid analgesia, and that women waited 13 minutes longer to receive treatment.
